Lifestyle, Nutrition, Physiology, Supplements
Insulin Resistance: Avoide/ Treatment/ Increas Sensivity
A Lethal Link Between Metabolic Disease and Heart Attack
Due to multimillion dollar advertising and marketing campaigns by the pharmaceutical industry, patients and physicians alike seem to associate heart attack and stroke risk only with cholesterol. Drugs that lower cholesterol (statins), have created a windfall of profit for pharmaceutical companies, with a single company’s statin drug often exceeding several billion dollars in annual sales. However, cardiovascular risk entails far more than just elevated cholesterol levels. In fact, the phenomenon known as insulin resistance offers a direct link between metabolic disease and cardiovascular risk, and is an often overlooked culprit underlying diabetes and heart disease. Learn how and why these two common diseases are intimately related and how to untangle them from your life. How are Blood Sugar and Plaque Related?Diabetes and heart disease are intertwined from the start, sharing a complex panel of hidden phenomena that lay the foundation for both conditions. If diabetes is present, heart disease is much more likely to develop. If heart disease develops, it is far more likely that diabetes will also.
The shared misfortune of diabetes and heart disease emerged with Dr. Steven Haffner’s 1998 report from the University of Texas that people with diabetes who do not have heart disease have the same risk for heart attack as people with established heart disease—the risk is one and the same.1 In 1999, the American Heart Association went on to label diabetes “a cardiovascular disease.” Since then, more studies have established this link. A 2001 study of people with stable heart disease but no previous history of diabetes found that approximately 50% of subjects had newly diagnosed disturbances of glucose metabolism (16% had full-blown diabetes and 36% had impaired glucose tolerance).2 Another recent study in persons hospitalized with more advanced, unstable heart disease symptoms (“unstable angina”) uncovered that 66% of those who met the criteria for diabetes were not diagnosed as such by their treating physician.3 In addition, the more extensive the heart disease identified, the higher the blood sugars tended to be. These insights provide us with strategies that could help diminish the likelihood of both diabetes and heart disease.
Insulin Resistance—Root of the ProblemThe majority of people with heart disease and diabetes have, often buried years earlier in their past, a pattern of poor responsiveness to insulin, or “insulin resistance.” Once this phenomenon becomes established, the stage is set. Insulin is the hormone that helps the cells and tissues of the body use glucose. An autoimmune process, whereby the body’s immune system attacks the insulin-producing cells of the pancreas, is the defect behind type 1 diabetes. This is a different process from so-called ‘adult-onset’, or type 2, diabetes.
Type 2 diabetes in adults represents a metabolic imbalance of both insulin secretion and insulin action at the cellular level, as opposed to the absolute deficiency of insulin observed with type 1 diabetes. In patients with type 2 diabetes, a number of factors lead to a poor response to insulin in muscle, fat, and liver. In essence, tissue cells become less responsive to insulin. This triggers the pancreas to overcompensate by producing greater quantities of insulin. Blood levels of insulin double, triple, even quadruple as the pancreas struggles to overpower the body’s poor responsiveness to insulin. This is the situation called “insulin resistance.” For reasons that have yet to be understood, an overworked pancreas cannot meet the increased demand for insulin for long. After just a few years, the insulin-producing beta cells of the pancreas begin to “burn out” and blood sugar rises. Rising blood sugar is therefore a sign of insulin resistance. Insulin resistance is present in 90% or more of people with diagnosed diabetes.4 In all practicality, adult-onset, or type 2, diabetes is synonymous with poor sensitivity to insulin. Insulin resistance is an underlying cause of a number of metabolic abnormalities that are grouped together in a condition called the metabolic syndrome. This disorder is associated with a host of undesirable consequences such as rising blood sugar, increased triglycerides, which lead to a reduction in beneficial high-density lipoprotein (HDL) and an increase in dangerous, small low-density lipoprotein (LDL) particles, greater risk for blood clotting, and high blood pressure.4,5 The list of metabolic phenomena triggered by insulin resistance should appear familiar—these are also risk factors for coronary atherosclerosis.4
More About Metabolic SyndromeMetabolic syndrome is known by a number of different names—insulin resistance syndrome, syndrome X, borderline diabetes, among others and is typically associated with increased triglycerides, reduced HDL, heightened inflammation, three-fold or greater risk of heart attack,6 greater risk for stroke, and diabetes.
Metabolic syndrome can drive the growth of atherosclerotic plaque even when everything else, like LDL, is corrected to perfect levels. Even with excellent LDL levels, for instance, hidden atherosclerotic heart disease can continue to grow at an alarming rate. The first step in guarding against insulin resistance and metabolic syndrome is to gauge one’s risk through simple tests such as triglycerides, insulin, blood pressure, HDL, C-reactive protein, and dehyroepiandro-sterone (DHEA). You and your doctor should suspect insulin resistance and metabolic syndrome if:
The likelihood of developing metabolic syndrome also escalates sharply above a body mass index (BMI) of 27. Keep in mind that these cut-offs are somewhat arbitrary and that lesser degrees of insulin resistance can be present before these cut-off points are fully reached. Some leading researchers advocate detecting risk of insulin resistance and metabolic syndrome by measuring waist size. If waist circumference is >35 inches in a female or >40 inches in a male, then metabolic syndrome is a high risk.7,8 Insulin Resistance and InflammationInsulin resistance is also associated with inflammation, as reflected by increased levels of the inflammatory markers nuclear factor-kappa B, interleukin-6, and C-reactive protein (CRP).5,9 C-reactive protein is the blood test that has emerged as a valuable tool to gauge hidden, imperceptible inflammation. Studies have consistently shown that the higher the CRP, the brighter the flame of inflammation that burns in the body and the greater the likelihood of heart attack and diabetes.10-12 In addition, insulin resistance triggers abnormalities in a recently recognized group of signaling molecules called adipokines.13 Fat cells, particularly those in the abdomen (“central obesity”), assume a life of their own and begin to act just like an independent new organ of the body, producing dozens of these unique substances. The adipokine, leptin, for instance, is produced by abdominal fat cells and causes white blood cells called macrophages to grab cholesterol particles, a phenomenon believed to add to coronary atherosclerosis. Tumor necrosis factor-alpha (TNF-alpha), another potent adipokine, activates inflammatory responses in vascular tissue and increases release of adhesive molecules, both of which add to atherosclerosis.5,14,15 Increased adipose tissue mass contributes to increased secretion of proinflammatory cytokines, especially TNF-alpha.15 Increasing Insulin Sensitivity and Reducing InflammationThe key to reducing or eliminating many of the threats of both metabolic syndrome/insulin resistance and heart disease is to chip away at the root cause of both and increase insulin sensitivity. Correct this fundamental defect and correction of multiple other phenomena will follow—HDL will increase, small LDL particles will be reduced, and triglycerides will plummet. The blood-clotting protein fibrinogen will also drop while physical stamina and energy will increase.
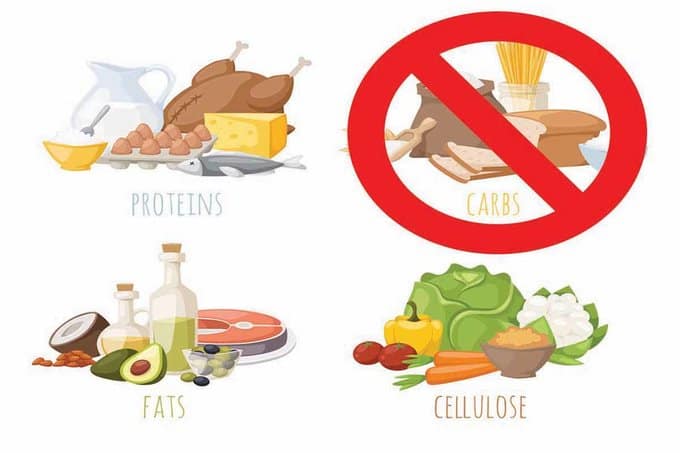
Likewise, hidden inflammation that fuels both heart disease and metabolic syndrome will be powerfully reduced. In most cases, insulin resistance, inflammation, and CRP can usually be reduced effectively and dramatically—usually to normal—just by using the nutritional supplements and lifestyle strategies discussed below. Furthermore, achieving glycemic control in patients with insulin resistance through lifestyle and nutritional interventions can effectively prevent or delay the development of cardiovascular problems and complications. As you will read, given the right kind of information, drugs are not always necessary, perhaps rarely. Lifestyle strategies that help correct insulin sensitivity, reduce hidden inflammation (CRP), and thereby contribute to reducing the likelihood of heart disease and diabetes include: Exercise. For improvement of insulin sensitivity, at least 30 minutes of physical activity per day is required for benefit, preferably 60 minutes. Also, the more frequent your efforts, the better. Exercise can scale down inflammation, as well. An Israeli experience in 28 patients with coronary heart disease showed that 12 weeks of aerobic exercise at 70–80% of maximum heart rate reduced CRP by 19% in non-diabetics and by 40% in diabetics.16 Strength training with weights or resistance machines also helps by increasing basal metabolic rate and accelerating fat loss. Twenty minutes twice a week of strength training can accelerate progress tremendously. Weight loss (if overweight). Weight loss yields the most dramatic effect of all for both improving insulin response and reducing inflammation. Weight reduction yields dramatic drops in CRP.17-19 The principal determinant is the amount of weight lost, not the means by which you achieve it.18–20 Healthy foods. Choose foods rich in soluble fiber and lower in glycemic load (i.e. the total amount of sugar and carbohydrate calories). The best foods are raw nuts and seeds, oat bran, lean proteins, and omega-3 fatty acids. Some dietary approaches may pack a greater effect than others (see below). Dietary strategies such as replacing saturated fat with healthy oils like olive, canola, and flaxseed (for monounsaturates); selecting lower glycemic-load foods such as lean proteins, whole grain products, and vegetables; and avoiding foods like processed white flour and white sugar-laden foods like cookies, crackers, candies, and cakes will help subdue inflammation and improve insulin response.21-23
The Mediterranean diet is one effective approach to improve insulin responses and reduce inflammation. The Greek ATTICA Study of over 3,000 men and women yielded 20% reduction of CRP in participants who most closely adhered to a traditional Mediterranean diet. The diet includes plentiful olive oil (a rich source of monounsaturated fat), vegetables and fruits, nuts, and fish, with little or no processed foods.24 Several other studies have demonstrated improvement in insulin responses and reduction of blood sugar on the Mediterranean diet.23,25,26 A major boost in soluble fiber intake may also increase success in reducing inflammation and insulin responses. David Jenkins, MD, PhD, DSc, at the Clinical Nutrition & Risk Factor Modification Center in Toronto has acquired a fascinating experience using an approach he calls “the dietary portfolio” of cholesterol-lowering foods. In one study, 46 participants followed a four-week nutrition program that added the following nutrients per 1,000 kcal of subjects’ total intake: 1.0 gram of phytosterols (high in plant sterols), 9.8 grams viscous, or soluble, fibers such as oat bran and oat products, barley, and psyllium seed, 21.4 grams soy protein, and 14 grams raw almonds. (An average 2,400 kcal diet would provide 2.4 grams phytosterols, 24 grams viscous fiber, 51 grams soy protein, and 34 grams almonds.) Participants averaged a fiber intake of 78 grams/day, which is five times more fiber than the average American consumes.27 A control group followed a very low saturated fat, dairy, and whole grain cereal diet, rather than foods containing viscous fibers and plant sterols.28 Dr. Jenkins’ dietary portfolio achieved an LDL reduction of 29% and a 28% reduction in CRP, compared with the control group who achieved only 8% reduction in LDL and 10% reduction in CRP. Another treatment group on the control diet received treatment with the cholesterol drug, lovastatin (Mevacor®), but performed no better than the dietary portfolio group.28 Dr. Jenkins’ dietary portfolio and other studies have also shown that abundant fiber intake, especially viscous or soluble fibers, slows the release of sugars into the bloodstream and thereby blunts excessive insulin responses. Improvements in insulin sensitivity and blood glucose responses have also been demonstrated in several other studies.29,30 Sleep. Chronic lack of a full night’s sleep impairs insulin function and contributes to the visceral (within abdominal contents) fat accumulation peculiar to metabolic syndrome.31 Maintaining seven to eight hours of sleep per night helps enhance insulin responses.31,32 Melatonin supplementation to restore normal sleep-wakefulness cycles may help improve metabolic syndrome and inflammation.33
Nutritional SupplementsThe following supplements can help reduce insulin resistance and inflammation in the body: Fish oil. Omega-3 fatty acids contained in fish oil help in numerous ways.34 Omega-3s effectively reduce the inevitably elevated triglycerides of metabolic syndrome, raise HDL, and reduce inflammation.35-38Of all their benefits, the triglyceride-reducing power of omega-3s represents their most powerful effect, which is likely responsible for the dramatic reduction in heart attack and stroke seen with supplementation.39-41 Approximately 1,400 mg eicosapentaenoic acid and 1,000 mg docosahexaenoic acid are recommended each day for maintaining a healthy heart. Chromium. Doses of supplemental chromium ranging from 200 mcg/day to 1,000 mcg/day improve blood sugar by enhancing the effects of insulin.42,43Chromium supplements also offer a useful adjunct to diabetic patients on sulfonylurea therapy, which is normally associated with weight gain when taken alone. In a recent study in adult diabetics, the usual weight gain seen with sulfonylurea therapy was significantly reduced by supplementing with chromium picolinate, 1,000 mcg/day.43 Other studies have demonstrated that chromium supplementation safely reduces cholesterol and triglyceride levels, and may reduce requirements for oral antidiabetes medication.44
White bean extract. This extract of the common white bean, Phaseolus vulgaris, is a starch blocker that blocks intestinal carbohydrate absorption by up to 66%. A recent randomized, placebo-controlled study showed that 445 mg of white bean extract twice daily in overweight adults led to 6.4 pounds of weight loss (while maintaining lean body mass) after 30 days compared with only 0.8 pounds in non-treated subjects.45 White bean extract also improves insulin responses by reducing sugar absorption and through weight loss.45 DHEA. When taken at bedtime, this adrenal gland hormone enhances mobilization of abdominal fat that contributes to metabolic syndrome, insulin resistance, and inflammation.46 Life Extension recommends the usual dose range for aging men and women is 15-75 mg daily. Ideally, DHEA-S blood levels should be obtained three to six weeks after dosing to assess individual response.46 Men and women with hormone-responsive cancers should only supplement with DHEA after clearance by their personal physician. Vitamin D. Numerous exciting reports about vitamin D’s myriad beneficial effects include recent observations that vitamin D deficiency contributes to insulin resistance and raises blood pressure (by increasing the blood pressure-raising hormone renin).47 Vitamin D deficiency is exceedingly common, particularly in northern climates, where up to 90% of people have moderate-to-severe deficiency. In sun-deprived climates, 1,000–4,000 IU/day may be required to raise blood levels to normal, occasionally more. Most people who lack sun exposure can safely take 2,000 IU/day.48 However, adequate sun exposure does not necessarily guarantee optimal vitamin D levels.49 Vitamin D status can be assessed by having one’s blood tested. Optimal levels are considered to be in the range of 30-50 ng/mL (75-125 nmol/L) of 25-hydroxyvitamin D in the blood. (Discuss vitamin D supplementation with your doctor if you have kidney disease, kidney stones, or a history of high calcium levels.) Vitamin D is also gaining recognition as a crucial modulator of inflammation. A University of London study demonstrated a dramatic reduction in the inflammatory proteins CRP and matrix metalloproteinase (MMP), after supplementation in 171 healthy adults, with a startling 68% reduction in MMP.50 Magnesium. This mineral is needed for more than 300 biochemical reactions and is recognized as an important mediator of insulin action and in reducing inflammation. In several studies, daily oral magnesium supplementation substantially improved insulin sensitivity by 10% and reduced blood sugar by 37%.51-53 The Women’s Health Study including nearly 12,000 participants showed that people who fail to take the recommended adequate intake of magnesium of 320-420 mg/day are more prone to have both metabolic syndrome and increased CRP.54Improved sensitivity to insulin generated by magnesium replacement can dramatically reduce triglycerides by as much as 75 mg/dL.53 Reduced triglyceride availability, in turn, reduces the triglyceride-rich particles, very low-density lipoprotein (VLDL) and small LDL, which are powerful contributors to heart disease. Magnesium supplementation can also raise levels of beneficial HDL.55,56 Magnesium deficiency is common not only from a dietary standpoint, but is also becoming an even larger issue as people turn to bottled water, which contains hardly enough magnesium, and as municipal water treatment more intensively “softens” its water by removing magnesium. Even the federal government admits that many Americans do not obtain the recommended amount of magnesium, which is 320 mg/day for women and 420 mg/day for men.57 Magnesium supplementation is therefore a basic requirement for health for most people. (Discuss this with your doctor if you have kidney disease or electrolyte disorders.) Flavonoids. Naturally occurring flavonoid compounds are important for suppressing inflammation. Emerging research suggests that some flavonoids also enhance insulin response and reduce insulin resistance. Of the thousands of known flavonoids identified, several, including polyphenols and resveratrol, stand out for these benefits. Polyphenols derived from green tea, cocoa, and apples are emerging as powerful facilitators of insulin responses as well as being potent anti-inflammatory compounds.58-60 A study comparing the effects of dark chocolate, containing beneficial cocoa polyphenols, with white chocolate (non-cocoa), 100 grams per day for 15 days, showed that only dark chocolate improved insulin sensitivity.61 Another study in 10 healthy volunteers showed that 37 grams of dark chocolate (containing 148 mg of procyanidins) yielded a 29% decrease in inflammatory leukotrienes and a 32% increase in the anti-inflammatory prostacyclin compared with subjects who received chocolate containing only 33 mg of procyanidins.58 This net decrease in the plasma leukotriene-prostacyclin ratio, a measure of proinflammatory-anti-inflammatory eicosanoid balance, dissipated six hours after subjects ingested the chocolate, suggesting that consumption of flavonoid sources several times a day is more likely to yield maximum benefit.58 Cocoa polyphenols also work in synergy with beta glucans, which offer an excellent source of low-glycemic carbohydrates. Beta glucans are an excellent form of soluble dietary fiber that help modulate the body’s response to carbohydrate-containing foods,62-64 promote satiety and weight loss,65 and lower CRP levels.66 Researchers have also found that cinnamon helps to diminish the dangerous after-meal surge in blood glucose,67 due to water-soluble polyphenols contained in this spice.68 Resveratrol, a flavonoid found in grape skins and concentrated in red wine, has also attracted a good deal of research attention. Red wine, 12 oz/day, has been found to improve insulin responses in people with diabetes. Resveratrol suppresses inflammatory mediators and powerfully inhibits matrix metalloproteinase, a trigger for atherosclerotic plaque rupture that results in heart attack and stroke.69 In data extrapolated from animal studies, resveratrol doses of at least 20 mg/day are necessary to protect against heart disease.70 A glass of red wine (about 6 oz or 180 mL) averages just 500 mcg of resveratrol.71In addition, resveratrol content in red wines varies enormously depending on type of grape, soil characteristics, methods of barreling, etc., but averages around only 2.5 mg/L.71 Non-drinkers and those seeking protection for a healthy heart can obtain resveratrol as a standalone supplement, or mixed with other flavonoids. The powerful antioxidant supplement, lipoic acid, is also a useful strategy to curtail inflammatory responses and improve insulin responses.72-78Although much of the research on lipoic acid 600-1,800 mg/day has focused on the improvement of painful nerve conditions associated with type 2 diabetes, lipoic acid also suppresses inflammatory mediators, such as interleukin-6 and plasminogen activator-1.79 Break the Insulin Resistance Connection and Lower Your Risk of Heart Disease and DiabetesChoosing low glycemic-load foods rich in soluble fiber, getting a full night’s sleep as consistently as possible, exercise, and taking nutritional supplements like fish oil, vitamin D (especially if you are sun-deprived), lipoic acid, magnesium, cinnamon, beta glucans, resveratrol, and polyphenols found in cocoa, green tea, and apples are part of a powerful integrative plan for breaking the insulin resistance connection. You can chart your progress by periodically measuring a variety of important metabolic and cardiovascular factors. You want to achieve:
If you have had a lipoprotein analysis, e.g., a VAP® (vertical auto profile) or NMR (nuclear magnetic resonance) test, reducing small LDL to <15% of total LDL can be a helpful secondary measure. Achieving a blood pressure of ≤130/85 mmHg is another important goal. Remember, decreasing heart disease risk is far more than simply taking a statin drug or making sure that your LDL is within an optimal range. By focusing on improving insulin sensitivity, you can help reduce the risk of heart attack and break the lethal connection between cardiovascular and metabolic diseases! |